The electrical signal is like the coxswain who gives the order to row. The individual rowers are like the heart muscle. Following the coxswain’s command each rower rows a stroke, all in unison, and their collective action pulls the boat forward. If the coxswain were to stop doing their job, and each rower were to row randomly on their own, all at different times and in different directions, then the boat wouldn’t go anywhere. A similar thing can happen in the heart if the electrical system goes offline and instead of generating a synchronized signal, simply generates jumbled, random electrical noise. Let’s look at what happens in the heart’s atriums, the two upper chambers of the heart, which are the first to squeeze during each heart beat. Normally, each muscle cell in the atriums squeezes simultaneously, like all the rowers rowing together in the crew boat. But when the electrical signal degenerates into only incoherent noise, then each muscle cell contracts randomly, at different times and different strengths. This results in the atria quivering continuously instead of a unified contraction. We call that quivering “fibrillating.” The atria are not contracting, they are just fibrillating. We call that atrial fibrillation.
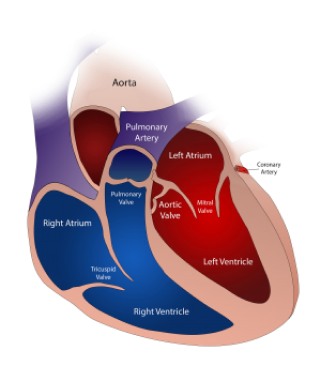
The heart’s atria, or upper chambers, are not responsible for the heart’s squeezing of blood out to the rest of the body – they do not cause the arterial pulsation. That is caused by the much larger and stronger lower chambers of the heart called the ventricles. The ventricles wait to beat until after the atria beat. The electrical signal passes through the atria, causing them to beat, and then continues to the ventricles, causing them to beat. During atrial fibrillation, the atria are simply fibrillating, not contracting. Our hearts have a failsafe mechanism which protects the ventricles from fibrillating during this situation. There is an electrical filter between the atria and the ventricles which prevents the disorganized electrical noise from propagating through to the ventricles and causing them to fibrillate as well. This filter is called the atrioventricular node, or AV node. The AV node blocks all the fibrillatory electrical signals and lets only a single unified signal through, so that the ventricles still contract together in a unified heart beat. But when the atriums are fibrillating, the electrical signal goes through the AV node to the ventricles at completely random intervals. This causes the ventricles to contract at random intervals. And that causes the arterial pulse to also become random. That is why if you feel the pulse of someone who has atrial fibrillation, you will feel the pulse to beat fast for a few beats, then slow, then fast, etc. And that is why AF is sometimes called an “irregular heart beat.” The heart’s squeezing of the blood is just as strong as it was before, because the ventricles are still squeezing the blood out normally with each beat. But the ventricular beats (and therefore the arterial pulsations) come at random intervals because of the electrical fibrillation in the atria.